Outcomes of force-directed balloon-assisted endoscopic Septoplasty: A retrospective analysis with a new technique and device
- David Joseph Dillard
- Dec 9, 2025
- 9 min read
Authors:
David Joseph Dillard2, Carlos Koudouovoh2, Vincent Lee1, Claire Barnes3, Roger Su2 James K. Fortson2
Key message
A new balloon-assisted, endoscopic septoplasty technique straightens a deviated nasal septum with statistically significant improvements in long-term nasal alignment and patient symptoms. By reducing flap dissection, this minimally invasive approach represents an alternative to traditional septum surgery that warrants further investigation.
Key words: Nasal Septum/surgery (septoplasty procedure), Nasal Obstruction (relief of nasal airway blockage), Balloon Dilation (use of balloon device for tissue expansion), Endoscopy (endoscopic surgical approach), Minimally Invasive Surgical Procedures (less extensive surgical technique)
Abstract:
Background:
Balloon-assisted endoscopic septoplasty using the ClearPath Nasal Balloon (CNB) offers a minimally invasive alternative to traditional septoplasty, aiming to reduce flap dissection, complications, and anesthesia time. This study aims to evaluate the efficacy and safety of this novel approach.
Methods:
This retrospective review analyzed 107 consecutive CNB septoplasty cases at Sleep and Sinus Centers of Georgia. Of these, 23 patients had pre- and post-operative CT scans available for assessment. Septal alignment was measured by the distance from the septum to the nasal sidewall at key anatomical landmarks, including the pyriform aperture (PYR), point of maximal deviation (PMD), and nasolacrimal ducts (NLD) using RadiAnt DICOM software. Postoperative CT scans were also assessed for complications. Statistical analysis was performed with paired t-tests.
Results:
Median values improved from 71 to 89 at the nasolacrimal duct (NLD), 36 to 83 at the point of maximal deviation (PMD), and 79 to 90 at the pyriform aperature (PYR), demonstrating statistically significant non-parametric gains. When a Wilcoxon Signed-Rank test for nonparametric data was used, all anatomical landmarks had statistically significant improvements. No major complications such as septal perforation or synechia were observed.
Conclusion:
The CNB technique appears to be a safe and effective minimally invasive option for septoplasty, providing significant radiographic improvements in septal alignment with no major complications in this cohort. However, larger studies with extended follow-up are needed to confirm these findings and determine the long-term durability and broader applicability of this novel approach.
Keywords:
Balloon-Assisted Endoscopic Septoplasty, ClearPath Nasal Balloon (CNB), septoplasty, nasal obstruction, deviated nasal septum, Nasal surgical procedures
Key points:
Significant findings of the study:
- The ClearPath Nasal Balloon (CNB) improved septal symmetry ratios at all landmarks: NLD 71 to 89, PMD 36 to 83, and PYR 79 to 90 (p < 0.05 for all).
- No major complications, such as perforations or synechia, were observed
postoperatively.
What this study adds:
- CNB-assisted septoplasty offers a minimally invasive alternative to traditional
techniques, reducing the need for extensive flap elevation.
- The CNB’s directional force component may enhance precision and safety, potentially improving patient outcomes and recovery times.
Main Text:
Introduction:
Septoplasty is a common otolaryngologic procedure, with ~250,000 surgeries performed annually in the United States. Traditional septoplasty requires mucoperichondrial flap elevation and resection of cartilage or bone, often necessitating suturing or packing and carrying risks such as perforation, hematoma, or synechia. Endoscopic septoplasty, developed in the 1990s, improved visualization and access but retained these limitations.
Hydrostatic balloon systems received FDA-approval in 2019 for endoscopic nasal surgery. The CNB incorporates a force-directed spatula that redistributes pressure, mobilizes the septum, and minimizes contralateral trauma. This design may reduce flap elevation and mucosal injury. This study evaluates CNB-assisted septoplasty outcomes and safety as a minimally invasive alternative to traditional septoplasty.
Methods:
This retrospective case series evaluated 107 consecutive patients who underwent CNB-assisted septoplasty over five years at Sleep and Sinus Centers of Georgia. The procedure was offered as a less invasive alternative to traditional septoplasty. Exclusion criteria included incomplete clinical, imaging, or survey data. Among 107 patients, 23 had both pre- and post-operative CT scans, and 43 completed SNOT-22 surveys.
Using a high-pressure (10 ATM) noncompliant balloon with a curved spatula, the CNB was sequentially dilated along the nasal floor, applying directional hydrostatic force over a 12x20 mm area for up to 10 sconds. CNB was used instead of conventional flap-based surgery to mobilize the bony septum. However, it does not address the cartilaginous septum or septal spurs. In these cases, limited mucosal flaps were required. Regarding complex septal deformities (“S” shaped), the CNB was used on each convex side of the deviation, often creating spurs which required removal due to excess bone length. CNB was not restricted to ethmoid plate deviations. Fractures were also induced along the vomer and maxillary groove.
CT scans were obtained preoperatively to evaluate sinus pathology, guide surgical planning, and assess causes of obstruction, and postoperatively in patients with persistent sinus complaints. CT scans were reviewed using DICOM. Septal alignment was measured at the PYR, NLD, and PMD. Although alignment varies by patient, the nasal tip and spine remain constant in an axial CT, ensuring consistency. Data were standardized as ratios, with 1.0 indicating midline symmetry.
Statistical analyses were performed using non-parametric methods (Wilcoxon signed-rank tests) due to non-normal data distribution. SNOT-22 scores measured qualitative outcomes. Interobserver reliability was assessed using Pearson correlation.
Results:
Of 107 patients undergoing CNB-assisted septoplasty, 23 had paired CT scans acquired at a median of 35 (range: 8-192) days preoperatively and 190 (31-1012) days postoperatively. No major intraoperative or postoperative complications or reoperations were identified. This includes perforation, hematoma, mucosal injury, infection, or conversion to traditional septoplasty.
At the NLD, median symmetry ratios improved from 71 to 89 (p=0.0042). Median PMD ratios improved from 38 to 81 (p=0.00005). PYR showed smaller gains, with median improving from 89 to 94 (p=0.02). Interobserver reproducibility was strong (Pearson r>0.98). See Tables 1-2 and Figures 3-5.
When stratified by baseline deviation at PMD, patients with greater initial septal deformity demonstrated the largest postoperative improvement. Overall, 16/23 (70%) achieved ≥30% improvement and no patients worsened (Figure 4).
Of the 107 patients in the cohort, 43 (40.2%) completed the Sinonasal Outcome Test-22 (SNOT-22) at their follow-up visit. Scores improved from 61 [51-72] to 46 [43-51], a 24.6% reduction (p=5.9x10-8). See Table 3 and Figures 6-7.
Discussion:
Endoscopic septoplasty has been shown to effectively correct a variety of septal deformities.1 CNB-assisted endoscopic septoplasty may represent a minimally invasive technique for addressing septal deviation, with observed improvements in septal alignment and patient-reported symptoms (median SNOT-22 improved from 61 to 46). These results appear to parallel outcomes reported in larger registries.2 For example, the Swedish registry found 81% of patients with severe nasal obstruction improved at 12 months, suggesting CNB-assisted methods may yield similar outcomes.2
Endoscopic septoplasty was popularized in the 1990s, and balloon sinus dilation introduced in 2006 provided a low-morbidity alternative to traditional sinus surgery (3-5). Balloon sinus procedures expanded rapidly, with Medicare data showing a 486% increase from 2011-2017, before plateauing after 2018 due to coding changes. (6,7) Continuing this trend towards minimally invasive techniques, the CNB’s non-compliant balloon applies up to 10 ATM of controlled hydrostatic pressure, while the contralateral curved spatula limits mucoperichondrial disruption, flap elevation, and nasal packing. The spatula redistributes pressure to reduce focal stress on mucosa (Figure 1). The technique has been performed in outpatient settings under local and general anesthesia.
Traditional septoplasty carries risks including septal perforation, cartilage necrosis, and orbital injury, and outcomes vary across patients and centers.8 In the UK National Comparative Audit, SNOT-22 scores improved from 42 to 25.5 in three months but with an 11.4% revision rate, while a Nordic registry reported ~25% persistent obstruction. (9,10) A Dutch study describes variable, yet notable, improvements.11 Hydrostatic balloon techniques have previously been shown to reduce tissue trauma and preserve cartilage viability, supporting their feasibility in pediatric and skull-base procedures.(12-15) In this cohort, CNB-assisted septoplasty demonstrated consistent median improvements across measured anatomic landmarks. Improved alignment may also enhance visualization and reduce complications in sinus and skull-base procedures, where limited visualization is a recognized contributor to adverse events.16 However, results should be interpreted cautiously: SNOT-22 reflects global sinonasal quality of life and thus may reflect symptoms beyond septal obstruction.
Conclusion:
Balloon-assisted endoscopic septoplasty using the CNB significantly improved septal alignment at key anatomical landmarks without postoperative complications. Outcomes were favorable, though interpretation is limited by the small sample size, retrospective design, and absence of a control group. Larger prospective studies, computerized modeling of CNB pressure distributions, and critical displacement angles observed in unguided balloon motion are needed to further substantiate these preliminary findings.
Word Count: 897 words
List of abbreviations
BMI- Body Mass Index
DICOM-RadiAnt Digital Imaging and Communications in Medicine
CNB- ClearPath Nasal Balloon
CT- Computed Tomography
NLD- Nasolacrimal Duct
PMD-Point of Maximal Deviation
PYR- Pyriform Aperture
SNOT-22- Sinonasal Outcome Test-22
References
Dell’Aversana Orabona G, Romano A, Abbate V, et al. Effectiveness of endoscopic septoplasty in different types of nasal septal deformities: experience with NOSE evaluation. Acta Otorhinolaryngol Ital 2018; 38: 323–330. doi: 10.14639/0392-100X-1067
Pedersen L, Schiöler L, Finjan S, et al. Prognostic factors for outcome after septoplasty in 888 patients from the Swedish National Septoplasty Register. Eur Arch Otorhinolaryngol 2019; 276: 2223-2228. doi:10.1007/s00405-019-05440-6
Kennedy DW. Functional endoscopic sinus surgery: technique. Arch Otolaryngol Head Neck Surg 1985; 111: 643-649. doi:10.1001/archotol.1985.00800120037003
Bothra R, Mathur NN. Comparative evaluation of conventional versus endoscopic septoplasty for limited septal deviation and spur. J Laryngol Otol 2008; 123: 737-741. doi:10.1017/S0022215108004192
Hopkins C, Browne JP, Slack R, et al. The national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Clin Otolaryngol 2006; 31: 390-398. doi:10.1111/j.1749-4486.2006.01275.x
Kasle DA, Torabi SJ, Narwani RV, et al. Medicare reimbursements for balloon catheter dilations among high-volume surgeons. JAMA Otolaryngol Head Neck Surg 2020; 146: 264-264. doi:10.1001/jamaoto.2019.4357
Liu DH, Torabi SJ, Bittner BF, et al. The impact of code bundling on Medicare volume and reimbursements within endoscopic sinus surgery. Otolaryngol Head Neck Surg 2025; 172: 356-359. doi:10.1002/ohn.987
Brenner MJ, Shenson JA, Rose AS, et al. New medical device and therapeutic approvals in otolaryngology: state of the art review 2020. OTO Open 2021; 5: 1-9. doi:10.1177/2473974X211507035
Hellgren J, Lundberg M, Rubeck N, et al. Unmet challenges in septoplasty: Nordic studies from a uniform healthcare and geographical area. Front Surg 2022; 9: 1061440. doi:10.3389/fsurg.2022.1061440
van Egmond MMHT, Rovers MM, Tillema AHJ, et al. Septoplasty for nasal obstruction due to a deviated nasal septum in adults: a systematic review. Rhinology 2018; 56: 195-208. doi:10.4193/Rhin18.016
Hur K, Kim M, Ference EH. Adverse events associated with balloon sinuplasty: a MAUDE database analysis. Otolaryngol Head Neck Surg 2019; 162: 137-141. doi:10.1177/0194599819884902
Pirsig W. Die Regeneration des kindlichen Septumknorpels nach Septumplastiken. Eine histologische Studie [Regeneration of septal cartilage in children after septoplasty. A histological study]. Acta Otolaryngol. 1975;79(5-6):451-459.
Nilsson W, Garst J, Kloens JS, et al. Use of balloon-assisted nasal access to augment endoscopic transsphenoidal approach: illustrative case. Case Rep Neurosurg 2022; 4: e2276. doi:10.3171/CASE2276
Lee D, Erickson A, You T, Dudley AT, Ryu S. Pneumatic microfluidic cell compression device for high-throughput study of chondrocyte mechanobiology. Lab Chip 2018; 18: 2077-2086. doi:10.1039/c8lc00320c
Aldueb R, Aljomah D, Almutawa H, Binnasser A. Septoplasty in a neonate using balloon dilation: case report and literature review. Acta Otolaryngol Case Rep 2024; 9: 12-15. doi:10.1080/23772484.2024.2331685
Hudgins PA. Complications of endoscopic sinus surgery. The role of the radiologist in prevention. Radiol Clin North Am. 1993 Jan;31(1):21-32. PMID: 8419976.
Figures:
Figure 1: ClearPath Nasal Balloon Model Diagram
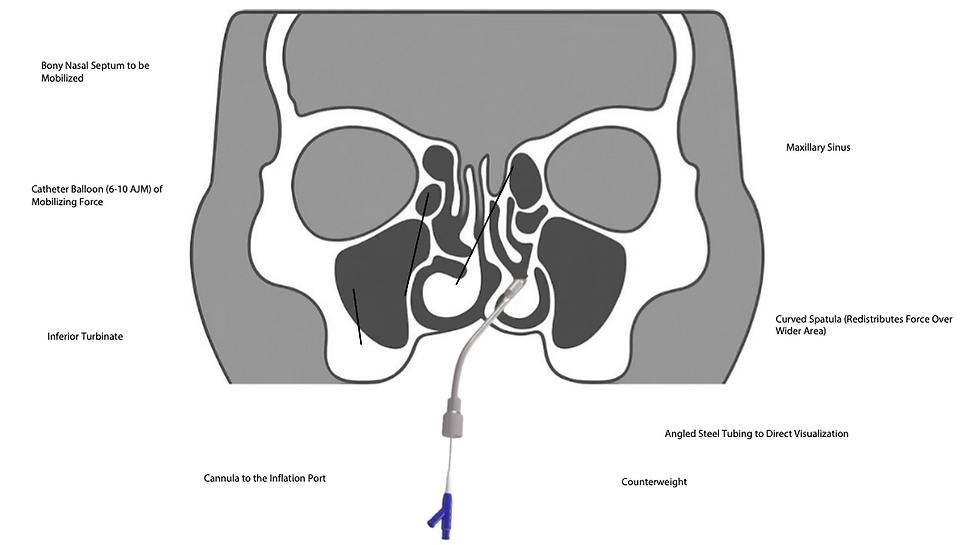
Figure 1 Legend: This diagram of the ClearPath Nasal Balloon (CNB) design for force-directional septal realignment. The shaped distal ‘spatula’ distributes balloon pressure evenly across the targeted bony septum, thereby allowing the surgeon to mobilize the septum while simultaneously minimizing unintended stress on adjacent lateral nasal structures. An angled steel shaft optimizes endoscopic visualization and serves as a counterbalance. The integrated cannula connects to the inflation port to allow controlled balloon expansion.
Figure 2: Pre-Operative and Post-Operative Axial CT Shows Septal Deviation at PMD

Figure 2 Legend: Pre-operative (left) CT scan shows significant septal deviation with a PMD of 65.60 mm from the midline. Post-operative (right) scan demonstrates improved septal alignment following CNB-assisted septoplasty.
Figure 3: Pre-Operative and Post-Operative Coronal CT Shows Septal Deviation at PMD

Figure 3 Legend: Pre-operative (left) CT shows septal deviation, while post-operative (right). Coronal CT images demonstrating preoperative (left) and postoperative (right) measurements at the point of maximal deviation (PMD). All measurements were obtained at a consistent anatomic level using a fixed reference point at the tip of the nasal spine or cartilage tip of the nose. Values were converted to ratios, with 1.00 indicating perfect midline symmetry, to allow for direct comparison between time points. CT demonstrates a 38% improvement in alignment after CNB-assisted septoplasty.
Figure 4: Post-Operative Septal Alignment Stratified by Baseline Deviation Severity

Figure 4 Legend: Post-operative septal alignment stratified by baseline deviation severity. Severe deviations (>10 mm) demonstrated the largest proportional correction, though all groups showed significant improvement
Figure 5: Comparison of Pre- and Post-Operative Symmetry Ratios for Nasolacrimal Duct and Point of Maximal Deviation

Figure 5 Legend: Pre- and post-operative symmetry ratios for the nasolacrimal duct and point of maximal deviation. Endoscopic septoplasty yielded improved mean ratios and reduced variability, reflecting enhanced nasal symmetry.
Figure 6: Wilcoxon Signed-Rank Test Demonstration High Correlation Between Observers Across Anatomic Landmarks

Figure 6 Legend: Inter-observer agreement on septal deviation measurements across anatomic landmarks. Strong correlations confirm reliability and reproducibility of the analytic method (bars represent Pearson Correlation Coefficients, r).
Figure 7: Summary of SNOT-22 Improvements Following Endoscopic Septoplasty Using the CNB

Figure 7 Legend: SNOT-22 outcomes before and after endoscopic septoplasty using the CNB technique. Post-operative scores showed reductions in symptom burden and variability demonstrating clinical efficacy.
Tables
Table 1: Summary of Efficacy Measurements of CNB in Endoscopic Septoplasty
Measurement | Pre-Op Measurement (Median [IQR]) | Post-Op Measurement (Median [IQR]) |
NLD Ratio | 71 [45-91] | 89 [78-96] |
PMD Median Ratio | 38 [25-50] | 81 [74-90] |
PYR Median Ratio | 89 [70-96] | 94 [85-98] |
Table 2: Summary of Wilcoxon Signed-Rank and Pearson Correlation Analyses for Symmetry Ratios for all Three Anatomic Landmarks
Anatomic Landmark | Pre-Op Median [IQR] | Post-Op Median [IQR] | Wilcoxon W-statistic (W-Critical = 55, ≅p<0.01) | Statistical Interpretation |
Nasolacrimal Duct (NLD) | 71 [45-91] | 89 [78-96] | 44 | Statistically significant |
Point of Maximal Deviation (PMD) | 38 [25-50] | 81 [74-90] | 5 | Statistically significant |
Pyriform Aperature (PYR) | 89 [70-96] | 94 [85-98] | 63 | Trend towards significance (p≅0.02) |
Table 3: SNOT-22 Outcomes Before and After CNB-Assisted Septoplasty
Wilcoxon Parameter | Statistical Output |
Pre-Operative Median [IQR] | 61 [51-72] |
Post-Operative Median [IQR] | 46 [43-51] |
W statistic (𝛂 =0.01, n=43, two tailed) | 24 |
Statistical Interpretation (W Critical = 138) | p=5.9 x 10-8 (statistically significant) |
Table 4: Baseline Demographic and Clinical Characteristics of Patients Undergoing CNB-Assisted Septoplasty (n=23)
Demographic Category | Value |
Median Age (years) | 40 [39-51] |
Sex (M/F) | Male: 52.2% |
BMI (kg/m2) | 26.4 kg/m² |
Smoking Status (yes/never/former) | Yes: 3 (13%); Never: 18 (78.3%); Former: 2 (8.7%) |
Nasal Obstruction Symptoms (>12 wks) | 65% (15/23 patients) |
Hypertension (BP >130/80) | 56 % (13/23 patients) |
Asthma | 8.7% (2 patients) |




Comments